IVF & Fertility
IVF & Fertility Treatments with Coastal IVF
Our clinic shares the same clinic and experienced team as Coastal IVF.
After a thorough assessment of your individual case, we will help determine which treatment is right for you.
Not only does this personalised approach save you costs, it saves you time and increases your chances of a successful outcome.
Below is a list of the assisted reproductive technologies (ART) offered at Coastal IVF
Ovulation Induction and Intra-Uterine Insemination (OI / IUI)
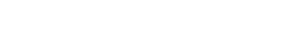
Stimulation of the ovaries (ovulation induction) to produce 1 to 3 eggs followed by the introduction of prepared sperm into the uterus at time of ovulation (intra-uterine insemination).
In Vitro Fertilisation (IVF)
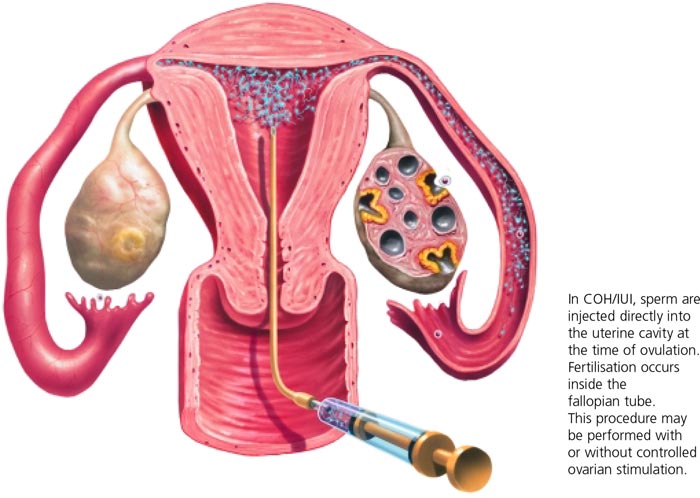
Literally meaning fertilisation in glass, in vitro fertilisation or IVF involves removal of an egg from the body and fertilisation in the laboratory to create an embryo, which is replaced into the woman’s uterus after 3-5 days.
Intra-Cytoplasmic Sperm Injection (ICSI)
An optional addition to IVF to assist fertilisation in cases where the sperm are unable to achieve this on their own.
Assisted Hatching and Pre-Implantation Genetic Diagnosis (AH / PGD)
Advanced form of assisted reproduction technology. Assisted Hatching involves creating a hole in the outer membrane of the embryo to assist the release of the embryo. Pre-implantation genetic (PGD) diagnosis is used to identify genetic anomalies in the embryo. This is useful to avoid certain genetic disorders and increase IVF success rates.
Sperm, oocyte and embryo freezing (Cryostorage)
Sperm, oocytes and surplus embryos can be frozen and stored for use in future treatment cycles.
We know this may seem overwhelming but we’re here to help you understand your options and make the process simple.
If you would like more detailed information on each option, simply take a look through the tabs below.
Treatments in Detail:
Ovarian stimulation
There are several methods or regimes of medication to assist in ovarian stimulation, some quite simple and others more complex.
The simplest option is to monitor the natural cycle and collect the egg as close to ovulation as possible.
The next step up is to mildly stimulate the ovary to produce a few eggs only – this is called minimal stimulation and is further expanded upon below.
Finally, there are a number of additional options where control is taken of the hormonal communication pathways between the pituitary gland and the ovary and the ovary stimulated to produce a larger number of eggs – these are called the; pill boost cycle, down regulation cycle and the GNRH Antagonist cycles all of which are further described below.
The pill boost cycle
The oral contraceptive pill is commenced when advised by the clinician. Each couple receive written instructions of their cycle plan. Synarel – A nasal spray is commenced which causes an initial surge of hormones from the Pituitary gland in the brain (which helps with the stimulation of the ovaries to produce more eggs). This then suppresses the pituitary to prevent a premature Luteinising Hormone (LH) surge which could ripen the eggs prior to egg retrieval. This enables us to control the development of eggs through use of daily injections of Follicle Stimulating Hormone (FSH). These medications are called Gonal F or Puregon, they are given as a subcutaneous injection which will be administered by yourself, partner or friend following instruction by the nurse coordinator. Both of these medications are continued until the eggs are ready for collection, determined by scanning and blood tests.
When the eggs appear ready for oocyte retrieval a hormone HCG (Human Chorionic Gonadotrophin) is given by injection which initiates ovulation 36 hours later. You will then attend the Day Surgery for your oocyte retrieval (egg pick-up).
Down regulation cycle
In this option, the nasal spray – Synarel – is commenced 2 weeks prior to the FSH injections.
When the eggs appear ready for oocyte retrieval a hormone HCG (Human Chorionic Gonadotrophin) is given by injection which initiates ovulation 36 hours later. You will then attend the Day Surgery for your oocyte retrieval (egg pick-up).
GnRh Antagonist
Cetrotide or Orgalutran can be used as an alternative to Synarel or Lucrin.
In this cycle, ovulatory response is initiated with FSH injections (Gonal F or Puregon) with early monitoring by ultrasound commencing on around day 6 of stimulation.
A second injection (the antagonist), Cetrotide or Orgalutran, will be introduced daily to prevent a premature LH surge once the leading follicle reaches 14mm or greater. When the eggs appear ready for oocyte retrieval a hormone HCG (Human Chorionic Gonadotrophin) is given by injection which initiates ovulation 36 hours later. You will then attend the Day Surgery for your oocyte retrieval (egg pick-up). See OPU and ET for diagrams.
One advantage of antagonist cycles is to decrease the risk of Hyperstimulation Syndrome, occasionally it can also be introduced when patients have had a poor response to other types of stimulation, although there is as yet not significant evidence from clinical studies to demonstrate greater effectiveness of these cycles.
Minimal stimulation or natural cycle
In this treatment program, follicular development is stimulated with the use of a medication usually taken between day 2 & 6 of a cycle.
Ovarian response is assessed with ultrasound on day 12 or 13 of the cycle with subsequent oocyte maturation induced with HCG.
In up to 30% of cycles adequate ovarian response will not be achieved or ovulation may occur prior to planned egg pickup.
This is because the natural feedback loop to the pituitary is still working and LH can be released prematurely.
Minimal stimulation cycles have a lower success rate than the above 2 FSH cycles but have the advantage of a reduced cost and lesser drug/medicinal intervention.
Ovulation Induction and Intra-Uterine Insemination
Key criteria for OI & IUI (Pro’s and Con’s):
- Female reproductive organs must be healthy
- Male must have good sperm count
- Mild ovarian stimulation using Clomiphene and monitoring of egg development using vaginal ultrasound, basal body temperature charts and urinary hormone tests
- Minimal laboratory involvement
- Low cost but success rates lower than IVF
- Once adequate follicular development has been determined, ovulation is triggered using a hormone and prepared sperm placed into the uterus.
We don’t push patients in to IVF treatment if your diagnosis suggest you may be more successful with a less invasive treatment.
We have one of the highest success rates with IVF, and we’re so confident in our proven processes that we also offer a second cycle guarantee – which means no out of pocket costs on a subsequent cycle if you need it.
Key requirements, pros and cons
- More demanding than OI / IUI
- Suitable for almost all forms of infertility
- Better success rates than OI / IUI
- More diagnostically informative than OI / IUI
- May need sperm injection to assist fertilisation
Did you know? Reproductive techniques were revolutionised by the birth of Louise Brown in 1978.
This was the world’s first IVF birth and Louise was delivered by a mother who did not have fallopian tubes.
This is the routine treatment now offered to patients whose tubes are not suitable for tubal surgery or if tubal surgery has failed.
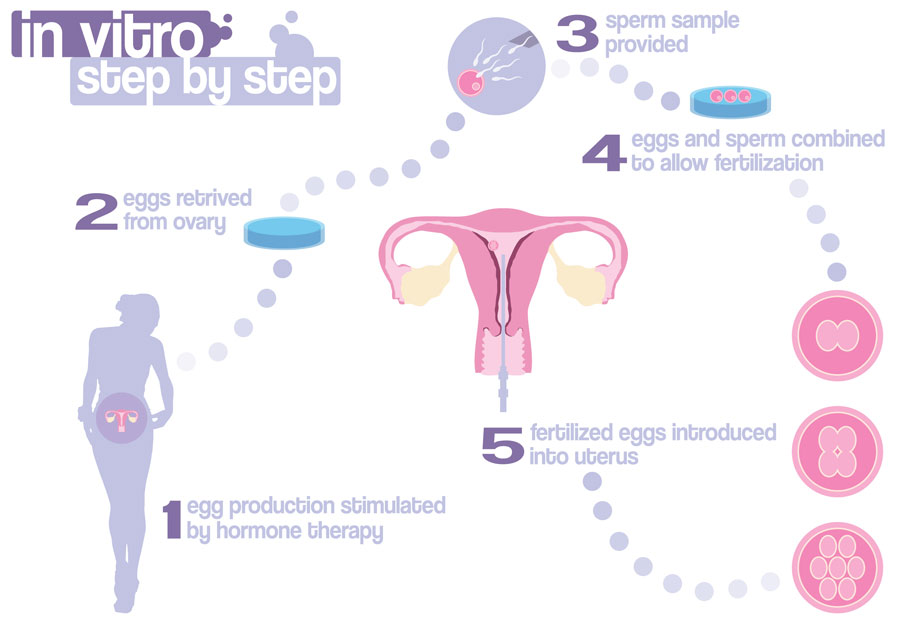
Oocyte pick-up and In Vitro Fertilisation (IVF)
Following stimulation of the ovaries with FSH injections, the eggs are collected from the patient via a vaginal ultrasound guided needle either under general anaesthesia or local anaesthetic. On average 11-12 eggs are collected after ovarian stimulation with FSH. The eggs are fertilised by the husband’s sperm and 1 to 3 of the resultant embryos are transferred to the mother’s uterus between 2 and 5 days following the egg collection. On average 65% percent of the eggs will be fertilised. The fertilised eggs are the grown (cultured) in the laboratory to either the day 2 / 3 stage known as cleavage stage embryos or to day 5/6 when the embryos have become blastocysts.
Stages of IVF treatment:
Cleavage stage embryo transfer (Day 2 or 3)
In general day 3 transfer is used as it allows more time for the faster developing embryos to become apparent, which assists in selecting embryos with a better potential. However, if there are only 1 or 2 embryos or the selection of embryos is clear earlier then embryos will be transferred on day 2. Surplus embryos can be frozen at this stage with a high degree of success (approximately 75% of embryos are suitable for transfer after thawing).
Blastocyst stage embryo transfer (Day 5 or 6)
Culturing the embryos for a further 2 or 3 days provides evidence of further developmental potential. This is useful in patients who have more than 3 embryos. Blastocysts can now be frozen with thaw survival rates as good if not better than cleavage stage embryos.
Other assisted reproduction methods
Various modifications to the conventional IVF method described above have been developed over the years and these are listed below. Some of these techniques have been shown to offer little advantage over conventional IVF or IVF supplemented with intra-cytoplasmic sperm injection and are now not commonly used. Whereas others are employed in specific circumstances only.
Gamete Intra Fallopian Transfer (GIFT)
GIFT is an appropriate therapy for some couples where there has been a past history of endometriosis and for unexplained infertility. Following stimulation of the ovaries with FSH injections, the eggs are collected via a vaginal ultrasound directed needle under general anaesthetic and while the patient is still asleep, 2 or 3 eggs are transferred to the mother’s tubes via a laparoscopy with semen from the husband for fertilisation then to occur in the tubes.
Pronuclear Stage Transfer (PROST)
PROST is a step further than GIFT in that fertilised eggs are place in the woman’s tubes one day after egg collection. This is particularly appropriate where there is a male factor and if there is some concern that fertilisation may not occur. The down side is that the woman requires 2 anaesthetics within 24 hours and is a technique now rarely used as it does not seem to improve the pregnancy rates compared to uterine embryo transfer in our experience.
Tubal Embryo Stage Transfer (TEST)
With the TEST procedure the embryos are placed into the fallopian tubes on the 2nd day after egg collection. The woman needs an anaesthetic for this transfer. Again this is rarely used, as we cannot demonstrate an improved pregnancy rate to justify the administration of two anaesthetics.
GIFT, PROST and TEST procedures are not commonly used these days.
Key benefits
- Used to assist fertilisation in cases where this cannot be achieved using conventional in-vitro fertilisation techniques, e.g low sperm count, poor sperm motility or with testicular sperm in instances where a vasectomy has been previously performed.
- A single sperm is captured using a fine glass needle and injected into the egg
- Fertilisation and pregnancy rates are comparable to conventional IVF methods
- This service is now covered by a Medicare rebate
This is a sophisticated technique, which involves the collection of an individual sperm and the injection of that sperm into an individual egg to obtain fertilization.
Any resultant embryos can be transferred to either the tube or the uterus. It is important to realise that a small percentage of men with defective semen assessments have an underlying chromosome disorder with the possibility of this affecting any offspring.
There can be a role for chromosome studies and genetic counselling in these individuals.

It is possible under local anaesthetic to extract sperm directly from the testicle using a fine needle biopsy technique and to then combine this with the ICSI technique to achieve fertilisation.
This can enable some couples, who would otherwise need donor sperm, to achieve a pregnancy with the genetic material of both partners.
The male requires initial investigations to see if this is an appropriate procedure for him, a physical examination and a hormonal profile being obtained.
There may also be a role for chromosome analysis and/or genetic counselling.
This technique can be offered to men following vasectomy if reversal is not a preference.
This is the biopsy technique of choice in men with obstructive azoospermia and replaces the more invasive open biopsy technique. It has a very low complication rate and a rapid recovery period.
Sperm and embryo freezing (cryopreservation) and storage
Key benefits
- Sperm freezing and storage can performed as a back up to using fresh sperm, such as when a husband’s work commitments prevent him from being available to provide a fresh sample. It also a useful backup technique for husbands who may find it difficult to produce a sample on the day of egg pick-up.
- After a stimulated ART cycle there may be surplus embryos. These can be cryopreserved and stored for use in a future cycle.
Frozen Embryo Transfer (FET)
Many reproductive techniques result in the development of more embryos than can be safely transferred in one treatment cycle. It is possible to freeze embryos and to thaw them at a later date for transfer to the patient. This has a slightly lower pregnancy rate than fresh embryo transfer but negates the need for a woman to go through a full treatment cycle to have another chance of achieving a pregnancy. The embryos are transferred to the uterus without an anaesthetic in a hormonally controlled cycle. There has not been shown to be any increase in foetal abnormalities using frozen embryos. Embryos can be frozen up to 6 days after insemination. To be suitable for freezing, embryos must be growing at the expected rate and have few fragments between the cells of the embryos. If only one embryo is frozen from the original cycle, it is recommended that further IVF cycles are undertaken in order to have sufficient embryos for subsequent thawing and transfer.
If donor gametes are involved, embryos from different donors cannot be transferred together. It is important to be aware that approximately 75% of frozen embryos survive thawing in a condition which is suitable for transfer. This can be a very disappointing stage if you have had preparation for a frozen transfer cycle. The staff will be available to discuss this and support you and endeavour to provide the next step of your infertility care.
Long-term storage of frozen embryos is not recommended as a routine. The National Health and Medical Research Guideline recommend that embryos not be stored for longer than five years other than in specific circumstances.
Egg pick up and embryo transfer
Egg pick-up
For fully stimulated cycles this procedure is performed under a light general anaesthetic in the Day Surgery. You are able to go home that day. There may be some bleeding and discharge following this and some lower abdominal discomfort. Coastal IVF does offer patients egg pick up in the rooms under local anaesthetic – speak to the nurse coordinator for further information. Click here to see a diagrammatic representation of an egg being removed from the ovary.
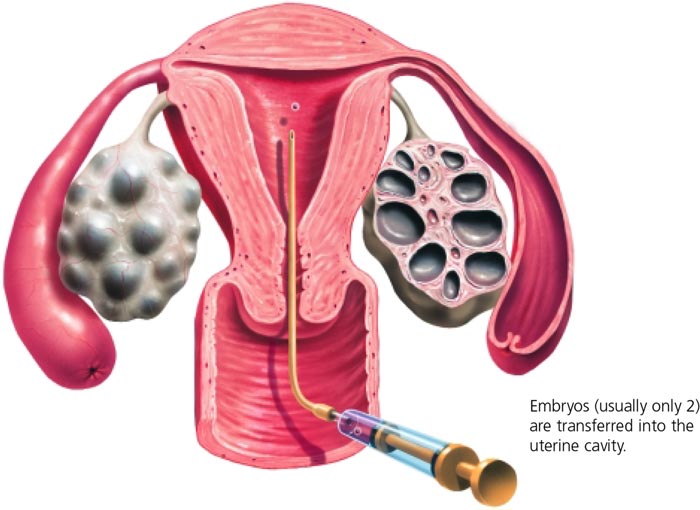
Embryo transfer
The embryo transfer is performed in the Coastal IVF rooms in the Clinical Procedures room adjacent to the IVF laboratory. The procedure involves placing a catheter loaded with the embryo/s into the uterus. The embryo/s are gently expelled from the catheter once it is in place. Click here to see a diagrammatic representation of an embryo transfer.
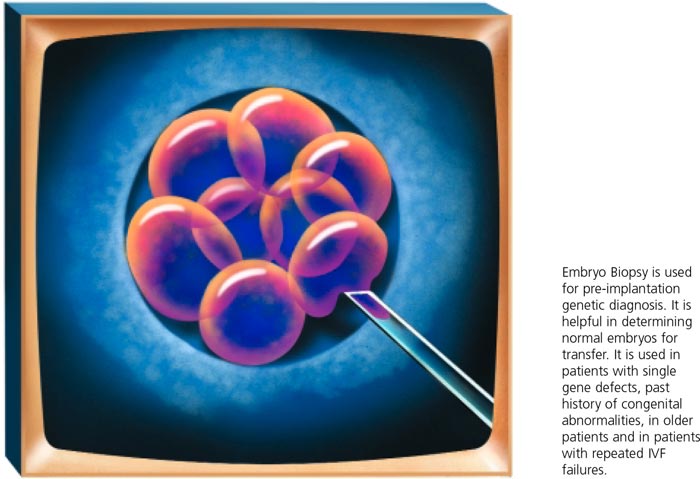
Assisted hatching and Pre-implantation Genetic Diagnosis
Key benefits
- Assisted hatching involves creating a hole in the outer membrane of the embryo to facilitate escape of the embryo.
Has not been shown to significantly improve success rates across the whole infertile population; however it appears to be of some benefit in selected groups of patients. - Pre-implantation Genetic Diagnosis (PGD) involves removal of one or two cells from an embryo and examination of the cells for specific chromosomal abnormalities. These can be for the presence or absence of the chromosome or for specific gene defects, called single gene defects. The embryos are biopsied in our laboratory and the cells sent away to reference genetic laboratories for analysis.
- Both techniques are employed only in selected cases.
What is Assisted Reproduction Technology (A.R.T.)?
A.R.T treatment comprises of 3 phases:
1) Ovarian Stimulation/ Ovulation
The ovulation induction or ovarian stimulation phase is where the growth of eggs (in the ovary) are tracked using blood tests (hormone monitoring) and ultrasound imaging. Medications are given to control ovarian physiology and stimulate the development of several eggs in a controlled manner. However, mild or no ovarian stimulation can be used if desired.
This phase lasts between 2 – 4 weeks depending on the treatment employed. The Assisted Reproduction Technology phase begins around mid cycle and can take up to 6-7 days in the case of blastocyct culture or 3-4 days for cleavage stage embryo transfer. This is where one of the following procedures will be employed.
2.1) Intra-Uterine Insemination (IUI)
2.2) IVF and Embryo Transfer (ET)
2.3) Frozen Embryo Transfer (FET)
These ART procedures are summarized below with more detailed descriptions of each technique.
Also see OPU and ET for information about the egg pick and embryo transfer.
3) Luteal Phase
The luteal phase corresponds to the second half of the menstrual cycle and involves the administration of injections or vaginal pessaries to assist the development of a suitable endometrium in the uterus for the embryo to implant into. Contrary to popular belief implantation of the embryo does not occur at the time of replacing the embryos into the uterus, but occurs a few days later. Pregnancy testing is performed at the end of this phase (16 days after egg pick-up).